IBS, SIBO, IBD ... Understanding chronic intestinal problems
IBS, SIBO, Crohn’s disease … There are many people who suffer regularly from intestinal problems. What are the symptoms and causes of these chronic conditions of the digestive system? And what can you do about them?

IBS (Irritable Bowel Syndrome)
What are the symptoms of IBS?
Irritable Bowel Syndrome (IBS), or functional colopathy, is a problem of the digestive tract which causes chronic abdominal pain. Manifesting as spasms or cramps, this pain is normally accompanied by uncomfortable bloating and dysfunctional transit (diarrhoea or constipation).
Between 5% and 15% of the population are thought to suffer from the syndrome. It is more common among women, with 2-3 females affected for every male (1).
This increased sensitivity of the gut causes considerable discomfort in those affected, both physiologically and psychologically. IBS may also result in headaches, fatigue, a sense of isolation, sleep problems, sexual dysfunction, etc. (2)
This functional bowel disorder is nonetheless benign: it neither increases the risk of bowel cancer nor appears to lower life expectancy.
Causes of IBS
Depending on the individual, IBS appears to be caused by:
- changes in intestinal motility (which make the bowel (large intestine) contract too strongly or weakly, either accelerating or decelerating the digestion of food);
- an initial episode of gastroenteritis which then goes on to damage the condition of the gut;
- hypersensitivity of the digestive system to bloating and intestinal gas;
- or deterioration of the gut microbiota which may increase the production of gas. This deterioration may be linked to excessive permeability of the intestine to bacteria (sometimes referred to as ‘leaky gut’).
Episodes of IBS are normally triggered by one or more of the following factors:
- eating a heavy or high-fat meal;
- consuming wheat, chocolate, milk, asparagus, beer, alcohol, etc.;
- eating too quickly;
- psychological factors such as stress, anxiety and depression...
How can IBS be managed?
There is currently no definitive treatment for IBS, but there are ways of reducing the frequency and intensity of symptoms. We would advise anyone suffering from IBS to consult their GP, who will be able to diagnose their problem and potentially prescribe suitable medication (anti-diarrhoeal drugs, laxatives, anti-depressants to block pain perception, etc.)
In addition, the general advice for IBS-sufferers is to:
- consume light, balanced meals on a regular basis, and to eat more slowly;
- drink plenty of water;
- identify foods that trigger their IBS and avoid them as much as possible. Common culprits are carbohydrates referred to as ‘FODMAPs’ (Fermentable Oligo-, Di-, Mono-saccharides And Polyols). (3-4) These carbohydrates , which feature widely in modern diets, are poorly absorbed by the small intestine and start to ferment, causing abdominal discomfort. A low-FODMAP diet involves reducing your consumption of foods such as peach, mushrooms, cabbage, leeks, salsify, beetroot, cream cheese, soya, honey, port and chewing gum. Conversely, some people have a specific sensitivity to dairy foods. Others find they have to avoid insoluble fibre (tomatoes, peppers, radishes, dried fruits, ...), which irritates the gut, and instead prioritise soluble fibre (oats, apples, oranges, onions ...) If you suffer from IBS, it’s a good idea to keep a food diary noting down any food that causes a problem, say two hours after ingestion. Note that it will probably take some time to arrive at the diet that works for you;
- supplement with vitamin D if you’re deficient. IBS is often associated with a lack of vitamin D (5) ;
- IBS-sufferers can also take a course of probiotics, which are a source of ‘gut-friendly’ bacteria (though you should always be guided by your doctor);
- in terms of natural ingredients, some studies recommend supplementing with lysine, bromelain, berberine and turmeric (6) ;
- if constipation is a problem, you should increase your intake of water and fibre, and perhaps supplement with psyllium (again, seek advice from your doctor first) (7) ;
- in general, IBS-sufferers should try to minimise any stress that may be triggering their flare-ups. Relaxation exercises such as deep abdominal breathing, or hypnosis are also an option (8). Those with IBS will also benefit from taking regular exercise as it will help maintain not just their gut but their overall health (9).
SIBO (Small Intestinal Bacterial Overgrowth)
What are the symptoms of SIBO?
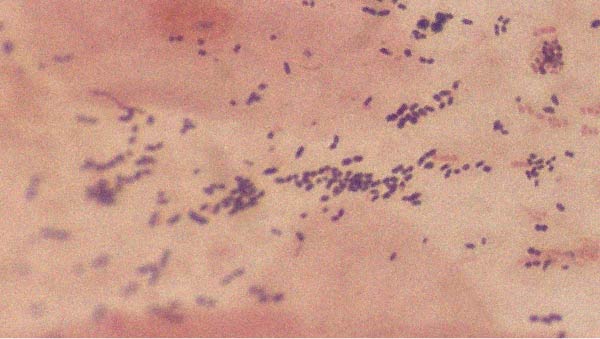
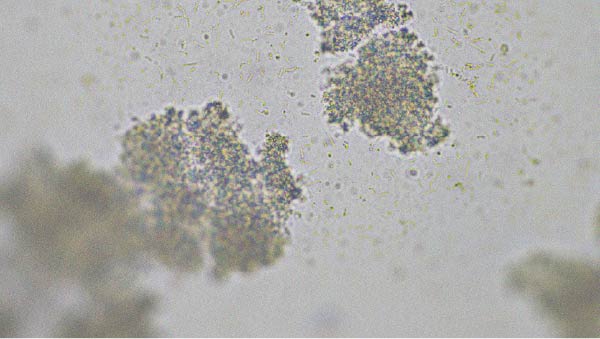
SIBO stands for Small Intestinal Bacterial Overgrowth. We know that the adult digestive system contains a wide range of microorganisms known as the gut microbiota. This microflora is essential not only for digestion but for our health in general. In someone with SIBO, the problem is that too many bacteria develop in the small intestine.
Their unwelcome presence triggers premature initiation of the food-fermenting process, which increases the production of intestinal gases: hydrogen, methane ... Like IBS, SIBO thus manifests in bloating, flatulence, digestive spasms, reflux or transit problems.
In addition, this disease usually causes deterioration to the intestinal wall, impaired carbohydrate digestion and poor absorption of nutrients (responsible for many deficiencies), as they get taken up by the bacteria. Again like IBS, SIBO can also give rise to a series of additional problems: chronic fatigue, depression, difficulty concentrating...
It’s important to say that this gut flora disorder is widely under-diagnosed, as there is little awareness of it among doctors, apart from in English-speaking countries (10). In France, it has been publicised by journalist and blogger Dora Moutot through her book À fleur de pet - le 1er livre sur la maladie des hyperballonnés qui ont le microbiote à l'envers (‘Fit to burst - the first book on the condition that causes extreme bloating in those with an upside-down microbiota’) (2019) (11).
Causes of this bacterial proliferation in the small intestine
SIBO may be initiated by:
- reduced secretion of gastric juices, which encourages the spread of bacteria. This decrease may be caused by certain drugs (PPIs and opioids);
- motility problems in the small intestine;
- a short intestine or as a result of surgery such as removal of the colon;
- insufficient chewing of food (12);
- consuming too much alcohol, coffee or fizzy drinks (13);
- stress, which affects intestinal motility and immunity;
- certain diseases are known to be associated with SIBO, such as auto-immune gastritis, chronic pancreatitis, fibromyalgia, cirrhosis and diabetes. It’s thought that 78% of IBS sufferers may also be affected by SIBO (14).
What can you do about SIBO?
Those who think they may have SIBO are advised to consult their doctor for a confirmed diagnosis and potential prescription of antibiotics to try and stem the spread of bacteria. There are also a number of natural approaches to consider:
- taking supplements can be helpful in resolving nutritional deficiencies caused by SIBO. Of particular note are vitamin A, vitamin B12, vitamin D, omega-3 and magnesium (15-16).
- some people may benefit from taking probiotics (again, consult your doctor first), though they are normally recommended following medical treatment in order to avoid adding bacteria to bacteria (17). Conversely, prebiotics must be avoided, as they could feed the bad bacteria;
- again, individuals suffering with constipation should increase their intake of fibre and water, and perhaps supplement with psyllium (18), as well as making sure they take exercise;
- in addition, alternative approaches to consider include the use of natural substances (some studies point towards the benefits of berberine, propolis, neem and the mushroom reishi), essential oils, and acupuncture... (19-21) ;
- a low-FODMAP diet, free from lactose or gluten, or high in meat and fats may also help. The paleo diet (which excludes grains, dairy products, sugar …) or intermittent fasting (where you fast for 16-24 hours) can also be effective for those with SIBO.
IBD: Crohn’s disease and ulcerative colitis
What are the symptoms of IBD?
Let’s end this overview of chronic intestinal problems by looking at IBD – Inflammatory Bowel Disease.
The term IBD covers two similar but distinct conditions: Crohn’s disease (or regional ileitis) and ulcerative colitis.
Both involve inflammation of the lining of the digestive tract. In ulcerative colitis, the inflammation more specifically affects the rectum and bowel. IBD can cause abdominal discomfort, recurrent diarrhoea or even anal abscesses.
It also increases the risk of developing colorectal cancer(22).
Causes of Crohn’s disease and ulcerative colitis
Incidence of IBD has been on the rise since 1945. This may be due to:
- genetic factors (there are potentially more than 150 genes that predispose to this disease);
- an increase in smoking (in the case of Crohn’s disease only);
- junk-food, pollution or excessive hygiene in childhood (though these various links have not yet been scientifically proven).
What can you do to address IBD?
Again, there is no real treatment for IBD. It is more a question of management:
- following diagnosis, anti-inflammatory medication is normally prescribed to try and prevent flare-ups. Immunomodulatory drugs, and even intravenous feeding, may also be recommended;
- if these prove unsuccessful, surgery may be considered after a few years. This consists of removing the most disease-damaged part of the intestine;
- IBD-sufferers will also find it helpful to note down the effects of the foods they eat and adapt their diet accordingly;
- and to compensate for the deficiencies caused by IBD, they can also choose to supplement with vitamins, zinc, iron and/or magnesium (for example, by taking a multivitamin supplement rich in vitamins and minerals) (23-25). As always, it’s best to consult a health professional for advice on the right supplements to take.
References
- Kim YS, Kim N. Sex-Gender Differences in Irritable Bowel Syndrome. J Neurogastroenterol Motil. 2018;24(4):544-558. doi:10.5056/jnm18082
- Sørensen J, Schantz Laursen B, Drewes AM, Krarup AL. The Incidence of Sexual Dysfunction in Patients With Irritable Bowel Syndrome. Sex Med. 2019;7(4):371-383. doi:10.1016/j.esxm.2019.08.010
- Moayyedi P, Andrews CN, MacQueen G, et al. Canadian Association of Gastroenterology Clinical Practice Guideline for the Management of Irritable Bowel Syndrome (IBS). J Can Assoc Gastroenterol. 2019;2(1):6-29. doi:10.1093/jcag/gwy071
- Varjú P, Farkas N, Hegyi P, et al. Low fermentable oligosaccharides, disaccharides, monosaccharides and polyols (FODMAP) diet improves symptoms in adults suffering from irritable bowel syndrome (IBS) compared to standard IBS diet: A meta-analysis of clinical studies. PLoS One. 2017;12(8):e0182942. Published 2017 Aug 14. doi:10.1371/journal.pone.0182942
- Caviezel D, Maissen S, Niess JH, Kiss C, Hruz P. High Prevalence of Vitamin D Deficiency among Patients with Inflammatory Bowel Disease. Inflamm Intest Dis. 2018;2(4):200-210. doi:10.1159/000489010
- Bundy R, Walker AF, et al. Turmeric extract may improve irritable bowel syndrome symptomology in otherwise healthy adults: a pilot study. J Altern Complement Med. 2004 Dec;10(6):1015-8
- Moayyedi P, Andrews CN, MacQueen G, et al. Canadian Association of Gastroenterology Clinical Practice Guideline for the Management of Irritable Bowel Syndrome (IBS). J Can Assoc Gastroenterol. 2019;2(1):6-29. doi:10.1093/jcag/gwy071
- Moayyedi P, Andrews CN, MacQueen G, et al. Canadian Association of Gastroenterology Clinical Practice Guideline for the Management of Irritable Bowel Syndrome (IBS). J Can Assoc Gastroenterol. 2019;2(1):6-29. doi:10.1093/jcag/gwy071
- Johannesson E, Ringström G, Abrahamsson H, Sadik R. Intervention to increase physical activity in irritable bowel syndrome shows long-term positive effects. World J Gastroenterol. 2015;21(2):600-608. doi:10.3748/wjg.v21.i2.600
- Mark Beattie, « Bacterial overgrowth », Oxford Medicine Online, septembre 2018 (DOI 10.1093/med/9780198759928.003.0040, lire en ligne [archive], consulté le 10 janvier 2019)
- https://www.youtube.com/watch?v=Gjsga5DlOZY
- Ardesia M, Villanacci V, Fries W. The agedgut in inflammatoryboweldiseases. Minerva GastroenterolDietol. 2015 Dec;61(4) 235-247. PMID: 26603728.,
- Gabbard, SL ,Lacy, BE , Levine, GM , Crowell, MD . The Impact of alcoholconsumption and cholecystectomy on small intestinal bacterialovergrowth. Dig Dis Sci. 2013.
- Ghoshal UC, Shukla R, Ghoshal J. Small intestinal bacterialovergrowth and irritable bowelsyndrome: a bridge betweenfunctionalorganicdichotomy. Gut liver. 2017;11(2):196-208.
- Andrea Michielan, Renata D’Incà, 2015, Review Article : Intestinal Permeability in Inflammatory Bowel Disease : Pathogenesis, Clinical Evaluation, and Therapy of LeakyGut,Volume 2015, Article ID 628157, 10 p., https://doi.org/10.1155/2015/628157
- PyndtJørgensen, B., Winther, G., Kihl, P., Nielsen, D., Wegener, G., Hansen, A., &Sørensen, D. (2015). Dietarymagnesiumdeficiency affects gutmicrobiota and anxiety-like behaviour in C57BL/6N mice. Acta Neuropsychiatrica, 27(5), 307-311. doi:10.1017/neu.2015.10
- Khalighi AR, Khalighi MR, Behdani R, et al. Evaluating the efficacy of probiotic on treatment in patients withsmall intestinal bacterial overgrowth (SIBO)--a pilot study. Indian J Med Res. 2014;140(5):604–608.
- Devinder Dhingra, Mona Michael, Hradesh Rajput et R. T. Patil, « Dietary fibre in foods: a review », Journal of Food Science and Technology, vol. 49, no 3, 12 avril 2011, p. 255–266 (ISSN 0022-1155 et 0975-8402, DOI 10.1007/s13197-011-0365-5, lire en ligne [archive], consulté le 10 janvier 2019)
- Yu ZC, Cen YX, Wu BH, et al. Berberine prevents stress-induced gut inflammation and visceral hypersensitivity and reduces intestinal motility in rats. World J Gastroenterol. 2019;25(29):3956-3971. doi:10.3748/wjg.v25.i29.3956
- Clark AK, Haas KN, Sivamani RK. Edible Plants and Their Influence on the Gut Microbiome and Acne. Int J Mol Sci. 2017;18(5):1070. Published 2017 May 17. doi:10.3390/ijms18051070
- Chang, C., Lin, C., Lu, C. et al. Ganoderma lucidum reduces obesity in mice by modulating the composition of the gutmicrobiota. Nat Commun 6, 7489
- Söderlund S, Granath F, Broström O, et al. Inflammatory bowel disease confers a lower risk of colorectal cancer to females than to males. Gastroenterology. 2010;138(5):1697-1703. doi:10.1053/j.gastro.2010.02.007
- Parian A, Limketkai BN. Dietary Supplement Therapies for Inflammatory Bowel Disease: Crohn's Disease and Ulcerative Colitis. Curr Pharm Des. 2016;22(2):180-188. doi:10.2174/1381612822666151112145033
- Li XX, Liu Y, Luo J, Huang ZD, Zhang C, Fu Y. Vitamin D deficiency associated with Crohn's disease and ulcerative colitis: a meta-analysis of 55 observational studies. J Transl Med. 2019;17(1):323. Published 2019 Sep 23. doi:10.1186/s12967-019-2070-5
- Ghishan FK, Kiela PR. Vitamins and Minerals in Inflammatory Bowel Disease. Gastroenterol Clin North Am. 2017;46(4):797-808. doi:10.1016/j.gtc.2017.08.011
2 Days
this company and its products are…
this company and its products are perfect: I have been their customer for three years , prices are reasonable for the high quality they offer , the products are of very good quality not just plainly "normal" , delivery is quite fast. we are very satisfied with them.
Gabriel Diacakis
2 Days
TOP service TOP products will buy again…
TOP service TOP products will buy again and again
PINOTTI Giorgio
5 Days
Trustworthy company with tested products
Trustworthy company with tested products
Trusted
9 Days
Efficiency and speed
Efficiency and speed
Cuccie
10 Days
GOOD BRAND IN FOOD COMPLEMENTS
GOOD BRAND IN FOOD COMPLEMENTS - SERIOUS WITH GOOD DOCUMENTS AND DETAILS SCIENTIST. AND SERIOUS HONNEST COMMERZIALISATION. I HAVE TRUST IN THEIR PRODUCTS.
FENOGLIO Guy
12 Days
Very good experience
Very good experience, the products arrived in time, in perfect condition and are good quality. Thank you.
GABI TIRCOCI
18 Days
very good expereince
very good expereince
Jelena Đaković
18 Days
Very good products.
Very good products.
Agnes BENDSAK
20 Days
Just OK
Just OK, ordering from company for many years and being safisfied
Lynn Mae
20 Days
Recomendo
Produtos encomendados são recebidos atempadamente e de acordo com o anunciado! Muito satisfeita!
Carla Sofia
21 Days
Everything is great!
Everything is great!
Jonas
26 Days
The delivery was fast and the product…
The delivery was fast and the product is great
SOMMARIVA Gianni
27 Days
Great service and lots of information
Great service and lots of information
Gabi
30 Days
Service Satisfaction
I’m satisfied with the service; it fulfilled what it set out to do.
Anfhony Abreu
33 Days
Original product and fast delivery
Original product and fast delivery. I haven't started it yet, but will do soon.
Vincenza Catania
of experience
your money back
##montant## purchase