In stock
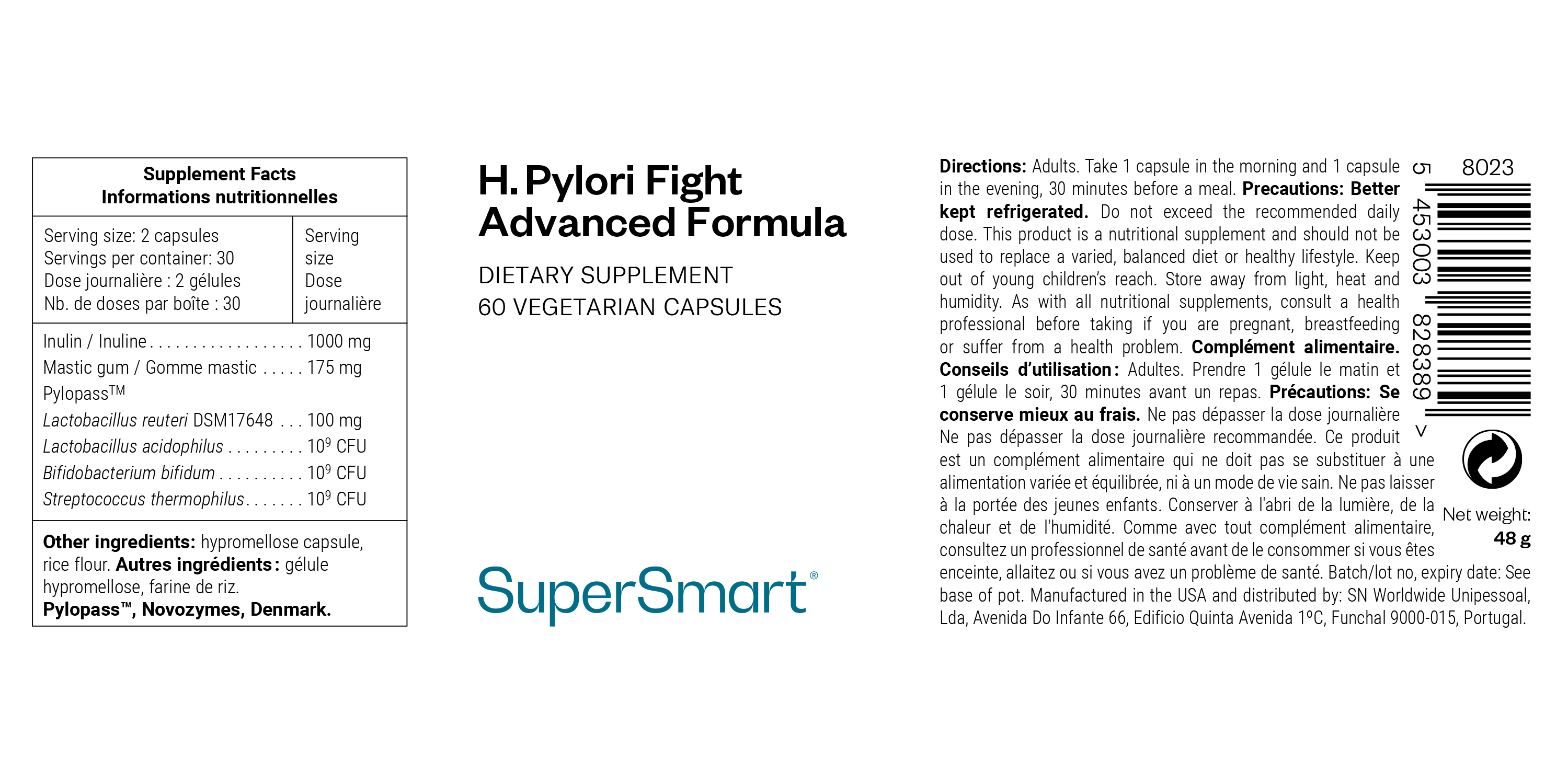
H. Pylori Fight Advanced Formula
Premium probiotic dietary supplement for Helicobacter pylori
Complete your selection
The ground-breaking synergy of H. Pylori Fight Advanced Formula reflects the latest scientific advances in the fight against the pathogenic bacteria Helicobacter pylori (or H. pylori). This ‘premium natural treatment’ is part of our Digestion and Oro-gastrointestinal health.
The premium formulation H. Pylori Fight Advanced Formula combines the excellent postbiotic Pylopass™ with 3 carefully-selected probiotics, as well as inulin and mastic gum, for unprecedented efficacy.
A ’premium, natural treatment’ with no antibiotics, targeted at Helicobacter pylori
An improved version of our famous H. Pylori Fight, the synergistic formulation H. Pylori Fight Advanced Formula combines all the most promising compounds for fightingHelicobacter pylori :
- Pylopass™ DSM17648: supported by more than 10 clinical studies, this patented postbiotic obtained from an inactivated probiotic strain of Lactobacillus reuteri, already a central component of H. Pylori Fight, is able to bind specifically to Helicobacter pylori bacteria. This co-aggregation significantly impedes its mobility and prevents it from adhering to the gastric mucosa. A study of 11 adults testing positive for H. pylori showed a reduction in bacterial load in 62.5% of participants after 28 days’ supplementation (1).
- Lactobacillus acidophilus: this lactic acid bacteria present in fermented dairy products helps promote a balanced gut microbiota. Studies also show it adheres to the gastric mucosa, preventing H. pylori from doing so itself. Other studies suggest that Lactobacillus acidophilus may also modulate the immune response and produce organic acids and other compounds able to inhibit the growth of H. pylori (2-3).
- Bifidobacterium bifidum: this probiotic strain, often used for treating gastritis associated with Helicobacter pylori, acts in a similar way to Lactobacillus acidophilus. By attaching to the lining of the stomach, it competes with Helicobacter pylori, thus reducing the number of potential attachment sites for this pathogenic bacteria. Bifidobacterium bifidum may also support immunity (4-5).
- Streptococcus thermophilus: this probiotic’s exopolysaccharides have also been shown to attach to the gastric epithelium (the first layer of the gastric mucosa which comes into contact with the contents of the stomach), and so these too reduce adhesion of Helicobacter pylori (6).
- Inulin: this fibre, typically described as a natural prebiotic, is found in various vegetables (chicory, artichoke, garlic, etc …). It supports the benefits of this microbiotic combo by ‘feeding’ the good bacteria and promoting their growth (7).
- Mastic gum: obtained from the mastic tree, this resin may, according to the scientific literature, have a bactericidal effect beneficial in reducing colonisation by Helicobacter pylori. Its effects are thought to be due to its acid fraction composed of terpene acids (8). It may also help to restore the gastric epithelium.
Reminder: what exactly is H. pylori bacteria?
Helicobacter pylori is a Gram-negative, spiral-shaped bacterium which colonises the inner lining of the stomach (9). Equipped with formidable adaptive mechanisms, it is one of the few pathogens able to survive in such an acidic environment. In particular, it produces an enzyme called urease which converts urea into ammonia, thus reducing stomach acidity and helping it proliferate in mucus (10). Once established, it will not go away by itself, persisting throughout life if not properly eradicated.
H. pylori contamination is extremely common, affecting around 50% of the world’s population (11). It usually occurs in childhood, primarily through direct contact with gastric secretions (regurgitation, vomiting …), or more rarely through stools, especially in developing countries with poor hygiene conditions. It can remain symptomless for long periods, but as we’ll see below, it can sometimes lead to serious complications.
Supplements to take alongside H. Pylori Fight Advanced Formula
To help restore the gastric mucosa, we’d suggest also taking DGL 500, a deglycyrrhizinated liquorice root supplement which supports gastrointestinal health by promoting mucus secretion, as well as Zinc L-Carnosine, as zinc helps protect cells against oxidative stress (21-22).
To relieve the gastric inflammation caused by H. pylori, you could also take turmeric (such as the product Super Curcuma which offers unrivalled absorption). Turmeric root has anti-inflammatory and antioxidant properties and has been used for thousands of years in Ayurvedic medicine to support digestive processes (23).
What is in H. Pylori Fight Advanced Formula
Any questions?
Our team of nutrition experts and scientists has the answers.
H. pylori causes chronic inflammation of the stomach (gastritis) which usually goes unnoticed (12): the vast majority of people infected will remain asymptomatic throughout their lives. Certain individuals, however, will suffer recurring digestive discomfort (pain and/or acid reflux, belching, nausea, vomiting, loss of appetite …) suggestive of H. pylori (13), though this not typical and is sometimes attributable to other causes.
In the absence of any emergency criteria, H. pylori infection can be ruled out by a blood test which detects IgG antibodies against the bacteria: a negative result automatically excludes contamination (16). There are two other lab tests that can be performed to detect the bacteria: the stool antigen test and the urea breath test (usually used at a later stage to monitor elimination of the bacteria following treatment) (17).
In the case of a positive result, a family history of stomach cancer or a particular clinical context (chronic dyspepsia, scheduled bariatric surgery, unexplained deficiency in vitamin B12 ...), an upper endoscopy or fibroscopy is the gold-standard diagnostic procedure (18). Taking and culturing a sample of cells from the stomach wall (biopsy) will confirm the presence of H. pylori and test its susceptibility to available antibiotics by establishing an antibiogram. Another advantage of an endoscopy is that it can reveal potential ulcerative or pre-cancerous lesions caused by the bacteria.
This product’s capsules are composed of HPMC (hydroxypropyl methylcellulose), a plant substance derived from cellulose. HPMC is widely used for medicines and dietary supplements. It contains no animal ingredients, is recognised as safe by health authorities and is considered more sustainable than synthetic alternatives.
Helicobacter pylori is all the more insidious because it develops quietly, often over several decades. Indeed, over the long term, it’s thought to cause lesions and peptic ulcers (affecting the stomach and/or duodenum, the first part of the small intestine) in 10% of those infected (14).
Very rarely (in around 1% of cases), carriers of the bacterium will go on to develop gastric cancer. Though this is extremely rare, H. pylori does appear to be responsible for almost 80% of stomach malignancies, hence the importance of establishing a treatment strategy as soon as possible after diagnosis to minimise this risk (15).
H. pylori is susceptible to only a handful of anti-infectious molecules. If the sensitivity of the bacterium could be tested, conventional treatment is based on a triple therapy combining a proton pump inhibitor (PPI) and antibiotics. Otherwise, an empirical quadruple therapy combining a PPI, antibacterial agents and/or bismuth salts is usually prescribed (19).
However, antibiotic treatment is far from infallible: it fails in 10%-20% of cases. As well as poor adherence to treatment, this failure seems to be new evidence of antibiotic resistance (20). The scientific community is also alarmed by the high primary resistance rate of H. pylori to certain treatments worldwide. The World Health Organization (WHO) has therefore classified this bacterium as a “priority pathogen for the research and development of new antibiotics”.
april 17 2025
Need help?
of experience
your money back
##montant## purchase